Abstract
Background
Low quality evidence exists to support an association between retinal vascular occlusion and thrombophilia. However, testing may be complicated by the impact of anticoagulants, hormone use and other factors on the results. Even when test results are interpretable, the implications for clinical decision-making are not established. We performed a retrospective chart review to assess patterns of test selection, result interpretation, and clinical outcomes in a cohort of patients who received thrombophilia testing after presenting to a tertiary care center for retinal vascular occlusion.
Methods
Eligible patients were >18 years with retinal vein occlusion (RVO) or retinal artery occlusion (RAO) and referred for thrombophilia testing by an ophthalmologist between 3/16/2011 and 3/22/2021 at the University of Washington. Electronic medical records were extracted for relevant clinical characteristics, test results, use of antithrombotic therapy, and recurrent arterial or venous events. Continuous variables are summarized by means and standard deviations or medians and range, as applicable. Categorical variables are described by proportions. Differences between groups were assessed using Student's t-tests and Fisher's exact tests for continuous and categorical variables, respectively. Analyses were conducted in R.
Results
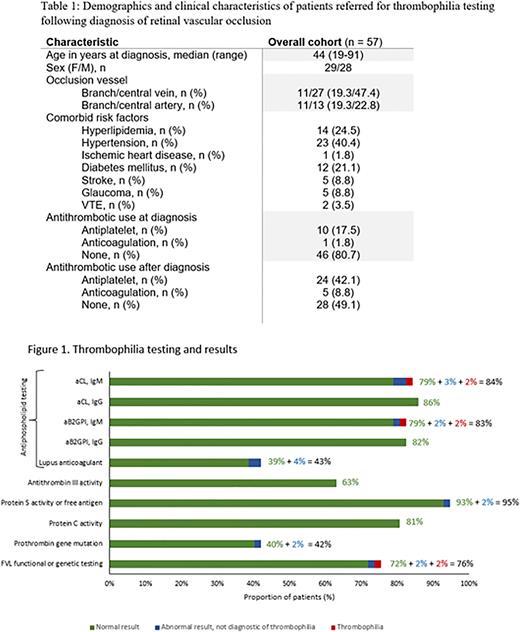
A cohort of 57 patients were identified, with median age of 44 years at diagnosis (Table 1). 38 (66.7%) presented with RVO and 23 (40.4%) presented with RAO, including 4 patients with concurrent RVO and RAO at diagnosis. Baseline characteristics were not significantly different between patients presenting RAO versus RVO, apart from a trend toward higher prevalence of stroke history in the RAO group (4/23 vs 1/38, p = 0.06).
Thrombophilia test selection varied: protein C activity was most commonly tested (80.7%) while activated protein C resistance (40.4%) was least commonly ordered (Figure 1). Among the 50 patients who received some combination of antiphospholipid antibody (aPL) testing, only 44% had all Sydney criteria aPL assays performed.
The underlying prevalence of thrombophilia was 3.5% (2/57). One patient was found to be homozygous for the factor V Leiden mutation (FVL) after presenting with a central RVO and 1 was diagnosed with antiphospholipid syndrome (APS) in the context of a branch RAO plus persistent positivity of anti-beta-2 glycoprotein I (IgM) and anticardiolipin (IgM) antibodies. Another 5 patients had abnormal test results that were not diagnostic of an underlying thrombophilia (1 heterozygous FVL, 1 heterozygous prothrombin gene mutation, and 3 positive aPL).
In total, 15 patients were initiated on low-dose aspirin following diagnosis, including the patient diagnosed with APS. Four patients were treated with anticoagulation, including the heterozygous FVL and heterozygous prothrombin gene mutation patients, who were placed on indefinite anticoagulation. The patient found to be homozygous for FVL briefly received prophylactic dosing of rivaroxaban before switching to low-dose aspirin due to side effects.
After a median follow-up of 3.1 years, 3 patients had recurrent events (1 RVO, 2 strokes). One developed recurrent stroke while taking rivaroxaban for atrial fibrillation, while the other 2 were not receiving antithrombotic therapy at the time of thrombosis recurrence.
Conclusion
A low prevalence of thrombophilia was observed in a young cohort of patients presenting with retinal vascular occlusion. Incomplete testing was common, including for antiphospholipid syndrome, which is associated with 2-fold increased risk of retinal vascular occlusion. Thrombophilia testing did not clearly aid in clinical decision making; the tests ordered and the actions taken based on the test result were inconsistent. Both patients identified to have underlying thrombophilia lacked other history of venous or arterial thromboembolism and ultimately opted against long-term anticoagulation. An additional 14 patients opted for antithrombotic therapy with low-dose aspirin after an entirely negative thrombophilia workup. Misinterpretation of test results likely led to inappropriate recommendations for indefinite anticoagulation in at least 2 patients. The utility of thrombophilia testing in retinal vascular occlusion is poorly studied. In this cohort, we found no evidence that such testing should influence clinical decision-making.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal